Sleep Less, Weigh More: Unraveling the Sleep-Obesity Connection in Adult
DOI:
https://doi.org/10.5281/zenodo.15308294Keywords:
Adult, Hormonal Regulation, Metabolic Health, Obesity, Sleep DurationAbstract
Background: Obesity is an increasingly complex and common global health problem, especially among adults. The aim of this scoping review is to examine the relationship between sleep duration and obesity in adults. Methods: A scoping review was conducted following the Joanna Briggs Institute (JBI) methodology guideline. Databases including PUBMED, ScienceDirect, DOAJ, and ResearchGate were searched in 2024 with the keywords "obesity AND sleep AND adults". Articles published between 2019 and 2023 that focused on observational studies. Results: Of the 2960 articles found, 7 articles met the inclusion criteria. A cross-sectional research design was used by 86% of the studies, while only 14% were enrolled in cohort studies. The majority of studies showed a significant correlation between short-term and long-term sleep duration and the likelihood of becoming obese. The assessment tools used were extensive and included interviews, questionnaires, and sleep monitors such as the Actiwatch Spectrum. The obesity assessment indicators used are Body Mass Index (BMI) and waistline. Conclusions: The review suggests that adults whose sleep is too short or too long are more likely to be obese. Lack of sleep can trigger hormonal changes, stimulate appetite, and result in obesity.
Downloads
References
Al Kibria, G. M., Swasey, K., Hasan, M. Z., Sharmeen, A., & Day, B. (2019). Prevalence and factors associated with underweight, overweight and obesity among women of reproductive age in India. Global Health Research and Policy, 4(1), 24. https://doi.org/10.1186/s41256-019-0117-z
Badan Penelitian dan Pengembangan Kesehatan. (2013). Riset Kesehatan Dasar (RISKESDAS) 2013. Laporan Nasional 2013, 1–384. https://doi.org/1 Desember 2013
Baez, A. S., Ortiz-Whittingham, L. R., Tarfa, H., Osei Baah, F., Thompson, K., Baumer, Y., & Powell-Wiley, T. M. (2023). Social determinants of health, health disparities, and adiposity. Progress in Cardiovascular Diseases, 78, 17–26. https://doi.org/https://doi.org/10.1016/j.pcad.2023.04.011
Caples, S. M. (2013). Sleep and Obesity. Encyclopedia of Sleep, 408–412. https://doi.org/10.1016/B978-0-12-378610-4.00341-7
Chaput, J.-P., McHill, A. W., Cox, R. C., Broussard, J. L., Dutil, C., da Costa, B. G. G., Sampasa-Kanyinga, H., & Wright, K. P. (2023). The role of insufficient sleep and circadian misalignment in obesity. Nature Reviews Endocrinology, 19(2), 82–97. https://doi.org/10.1038/s41574-022-00747-7
Chaput, J. P., Dutil, C., Featherstone, R., Ross, R., Giangregorio, L., Saunders, T. J., Janssen, I., Poitras, V. J., Kho, M. E., Ross-White, A., & Carrier, J. (2020). Sleep duration and health in adults: an overview of systematic reviews. Applied Physiology, Nutrition, and Metabolism = Physiologie Appliquee, Nutrition et Metabolisme, 45(10), S218–S231. https://doi.org/10.1139/apnm-2020-0034
Dhawan, D., & Sharma, S. (2020). Abdominal Obesity, Adipokines and Non-communicable Diseases. The Journal of Steroid Biochemistry and Molecular Biology, 203, 105737. https://doi.org/https://doi.org/10.1016/j.jsbmb.2020.105737
Hirshkowitz, M., Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C. A., Bruni, O., Doncarlos, L. L., Hazen, N. L., Herman, J. H., Katz, E. S., Kheirandish-Gozal, L., Neubauer, D. N., O’donnell, A. E., Ohayon, M. M., Peever, J. H., Rawding, R., Sachdeva, R. C., Setters, B., Vitiello, M. V, … Hillard, P. J. A. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1 1, 40–43. https://api.semanticscholar.org/CorpusID:205190733
Jakubiak, G. K., Osadnik, K., Lejawa, M., Kasperczyk, S., Osadnik, T., & Pawlas, N. (2021). Oxidative Stress in Association with Metabolic Health and Obesity in Young Adults. Oxidative Medicine and Cellular Longevity, 2021. https://doi.org/10.1155/2021/9987352
Kim, T. W., Jeong, J. H., & Hong, S. C. (2015). The impact of sleep and circadian disturbance on hormones and metabolism. International Journal of Endocrinology, 2015. https://doi.org/10.1155/2015/591729
Kolovos, S., Jimenez-Moreno, A. C., Pinedo-Villanueva, R., Cassidy, S., & Zavala, G. A. (2021). Association of sleep, screen time and physical activity with overweight and obesity in Mexico. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, 26(1), 169–179. https://doi.org/10.1007/s40519-019-00841-2
Li, N., Wang, R., Hu, P., Lu, W., Zhao, X., Wang, L., Song, M., Gao, Y., An, C., Bashir, S., & Wang, X. (2023). Effect of night shift work on metabolic syndrome in adults who suffered from earthquake stress in early life. Frontiers in Public Health, 11(July), 1–7. https://doi.org/10.3389/fpubh.2023.1139113
Lin, J., Jiang, Y., Wang, G., Meng, M., Zhu, Q., Mei, H., Liu, S., & Jiang, F. (2020). Associations of short sleep duration with appetite‐regulating hormones and adipokines: A systematic review and meta‐analysis. Obesity Reviews, 21. https://api.semanticscholar.org/CorpusID:219700766
Liu, S., Wang, X., Zheng, Q., Gao, L., & Sun, Q. (2022). Sleep Deprivation and Central Appetite Regulation. Nutrients, 14(24), 1–12. https://doi.org/10.3390/nu14245196
Loredo, J. S., Weng, J., Ramos, A. R., Sotres-Alvarez, D., Simonelli, G., Talavera, G. A., & Patel, S. R. (2019). Sleep Patterns and Obesity: Hispanic Community Health Study/Study of Latinos Sueño Ancillar Study. Chest, 156(2), 348–356. https://doi.org/10.1016/j.chest.2018.12.004
Macicame, I., Prista, A., Parhofer, K. G., Cavele, N., Manhiça, C., Nhachungue, S., Saathoff, E., & Rehfuess, E. (2021). Social determinants and behaviors associated with overweight and obesity among youth and adults in a peri-urban area of Maputo City, Mozambique. Journal of Global Health, 11, 4021. https://doi.org/10.7189/jogh.11.04021
Mahdieh Momayyezi, Hossein Fallahzadeh, Leila Fakhravari, M. M. (2021). The Association between Sleep Pattern with Lipid Profile and Obesity among Adults in Yazd: Cross-Sectional Analysis of Shahedieh Cohort Study. Journal of Nutrition and Food Security. https://doi.org/DOI https://doi.org/10.18502/jnfs.v7i3.10198
Medic, G., Wille, M., & Hemels, M. E. H. (2017). Short- and long-term health consequences of sleep disruption. Nature and Science of Sleep, 9, 151–161. https://doi.org/10.2147/NSS.S134864
Morales-Ghinaglia, N., & Fernandez-Mendoza, J. (2023). Sleep variability and regularity as contributors to obesity and cardiometabolic health in adolescence. Obesity, 31(3), 597–614. https://doi.org/https://doi.org/10.1002/oby.23667
Morin, V., Hozer, F., & Costemale-Lacoste, J.-F. (2018). The effects of ghrelin on sleep, appetite, and memory, and its possible role in depression: A review of the literature. L’Encéphale, 44(3), 256–263. https://doi.org/https://doi.org/10.1016/j.encep.2017.10.012
Mosavat, M., Mirsanjari, M., Arabiat, D., Smyth, A., & Whitehead, L. (2021). The Role of Sleep Curtailment on Leptin Levels in Obesity and Diabetes Mellitus. Obesity Facts, 14(2), 214–221. https://doi.org/10.1159/000514095
Parameswaran, G., & Ray, D. W. (2022). Sleep, circadian rhythms, and type 2 diabetes mellitus. Clinical Endocrinology, 96(1), 12–20. https://doi.org/10.1111/cen.14607
Kemenkes RI (2018). Basic Health Research (Riskesdas) 2018. Health Research and Development Agency.
Kemenkes RI (2007). RISKESDAS 2007.
Rodrigues, G. D., Fiorelli, E. M., Furlan, L., Montano, N., & Tobaldini, E. (2021). Obesity and sleep disturbances: The “chicken or the egg” question. European Journal of Internal Medicine, 92, 11–16. https://doi.org/https://doi.org/10.1016/j.ejim.2021.04.017
Safaei, M., Sundararajan, E. A., Driss, M., Boulila, W., & Shapi’i, A. (2021). A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Computers in Biology and Medicine, 136, 104754. https://doi.org/https://doi.org/10.1016/j.compbiomed.2021.104754
Tanvir, M., Abida, M., & Nazeer, M. (2023). A study of sleep duration, body mass index and blood pressure in an adult Kashmiri population. International Journal Of Community Medicine And Public Health, 10(12), 4684–4689. https://doi.org/10.18203/2394-6040.ijcmph20233763
Thapa, S., Ahmed, K. Y., Bizuayehu, H. M., Huda, M. M., Chalise, B., Bore, M. G., Belachew, S. A., Hassen, T. A., Amsalu, E., Shifti, D. M., Seid, A., Mesfin, Y. M., Tegegne, T. K., Dadi, A. F., Odo, D. B., Kibret, G. D., Ketema, D. B., Kassa, Z. Y., Anyasodor, A. E., … Ross, A. G. (2024). Trends and social determinants of the obesity epidemic among reproductive-age women in ten Asian countries. Scientific Reports, 14(1), 22545. https://doi.org/10.1038/s41598-024-73522-5
Vgontzas, A. N., Fernandez-Mendoza, J., Miksiewicz, T., Kritikou, I., Shaffer, M. L., Liao, D., Basta, M., & Bixler, E. O. (2014). Unveiling the longitudinal association between short sleep duration and the incidence of obesity: the Penn State Cohort. International Journal of Obesity, 38(6), 825–832. https://doi.org/10.1038/ijo.2013.172
von Schantz, M., Ong, J. C., & Knutson, K. L. (2021). Associations between sleep disturbances, diabetes and mortality in the UK Biobank cohort: A prospective population-based study. Journal of Sleep Research, 30(6), 1–7. https://doi.org/10.1111/jsr.13392
WHO. (2024). Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Yao, F., Ma, J., Qin, P., Tu, X., Li, X., & Tang, X. (2022). Age and Sex Differences in the Association of Sleep Duration and Overweight/Obesity among Chinese Participants Age above 45 Years: A Cohort Study. The Journal of Nutrition, Health and Aging, 26(7), 714–722. https://doi.org/https://doi.org/10.1007/s12603-022-1823-7
More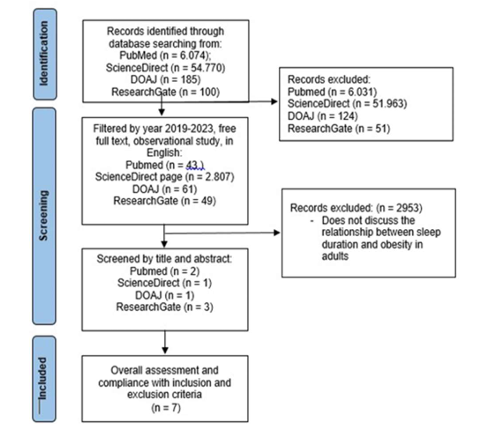
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Az’yan Nazwa Maharani Putri, Rahmah Dwi Yuliyanti, Almira Sitasari, Agus Wijanarka, Jutharat Attawet, Tri Siswati (Author)

This work is licensed under a Creative Commons Attribution 4.0 International License.